Mass Screening for Celiac Disease?
To screen or not to screen, that is the question!
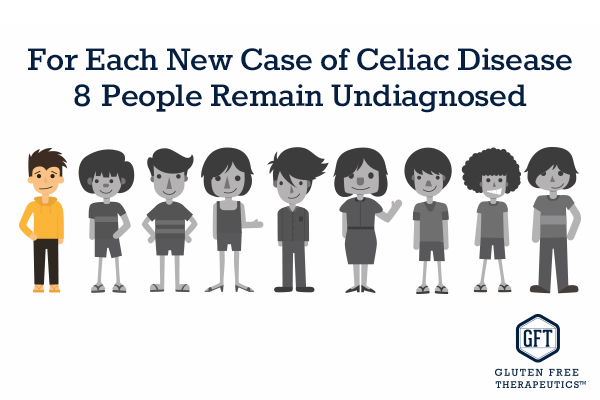
We have all heard the statistic that 87% of celiac patients go undiagnosed. So should celiac disease fall under mandatory mass screening guidelines?
Celiac disease is notoriously difficult to diagnose, and for every new case it is estimated that about 7 or 8 remain undiagnosed. Given the higher mortality and morbidity rates in undiagnosed patients, can the answer be mass screening? This would certainly detect every case, even before symptoms develop, but is it the best solution to get everybody checked for celiac disease? If not what is the solution to the diagnosis gap?
In 1968, the World Health Organization issued guidelines to determine which diseases should be checked with mass screening, but over 50 years later, researchers and physicians are still debating if these parameters can be applied to celiac disease.
Yes or no: the arguments
In fact, only a minority stands by a mass screening of the general population. The condition does cover several criteria defended by the WHO to justify mass screening, including relatively high prevalence and difficult diagnosis, as well as available tests and potential complications if not treated. The problem with this approach is that it will inevitably lead to conflicting results when faced with the borderline patients. For example, it’s possible for patients to have positive celiac serology, but a perfectly normal bowel after biopsy. This leaves these patients in “limbo”, with only half-diagnosis. Does this mean they would have to repeat the biopsy? When? Are they at risk of complications? Should they follow a gluten-free diet? These issues also raise other important questions about when to conduct the screening: could the best way be to screen at a young age and offer regular check-ups to those with a genetic predisposition or wait until the disease has had time to develop?
Currently, as most of these questions remain unanswered, most believe we don’t know enough about the condition to benefit from mass screening. This is also the view of the National Institutes of Health and many other institutions around the world. One of the main obstacles is a poor adherence to a gluten-free diet, which can be expensive and difficult to get. Reality is asymptomatic patients fail to see the benefit of following a strict diet, offsetting any advantages of mass screening. In addition, being diagnosed with celiac disease can decrease quality of life and some screen-detected patients regret finding out about their condition.
The best solution: screen high-risk groups
At this stage, although still pursuing the idea of mass screening, most researchers agree that screening only high-risk groups is the best solution. These groups include, for example, first-degree relatives and patients with other autoimmune conditions. The idea of catching every single case of celiac disease may be appealing, but further research is needed to evaluate the extent to which treatment of screen-detected celiac disease patients actually reduces long-term negative health consequences or whether imposing a gluten-free diet would inflict unnecessary strain on these patients.
 This original article is made possible by Gluten Free Therapeutics. Our mission is to educate, inform, and provide the most effective nutritional products possible to allow those with celiac disease and serious gluten intolerances to heal their bodies. CeliVites complete line of superior gluten free supplements includes multivitamin/multimineral supplements, iron supplements, and calcium supplements for people living with celiac disease. All CeliVites products are designed to help you heal, restore and rebuild your body, because going gluten free isn’t enough!
This original article is made possible by Gluten Free Therapeutics. Our mission is to educate, inform, and provide the most effective nutritional products possible to allow those with celiac disease and serious gluten intolerances to heal their bodies. CeliVites complete line of superior gluten free supplements includes multivitamin/multimineral supplements, iron supplements, and calcium supplements for people living with celiac disease. All CeliVites products are designed to help you heal, restore and rebuild your body, because going gluten free isn’t enough!
Comments ()













I understand that Europe does mass screening. I feel that if one eats produce from the earth and has no food with preservatives, one is gluten free.
Great point Norma, we base our meals around fresh organic foods, even meat has to be organic. No processed or boxed foods. It is easier than it sounds. Thank you for sharing.
I have a personal history of ulcerative colitis and now IBS I am now back on bentyl and taking 5 mg prednisone daily for a flare up of rheumatoid arthritis. My daughter (25 Y.O) has been diagnosed with IBS (colitis/possible celiac disease) What should i be doing to help improve my health. I try to watch my diet however, I am unable to eat fresh fruits and vegetables. I am unable to eat any kind of cabbage, broccoli, spinach, cauliflower…