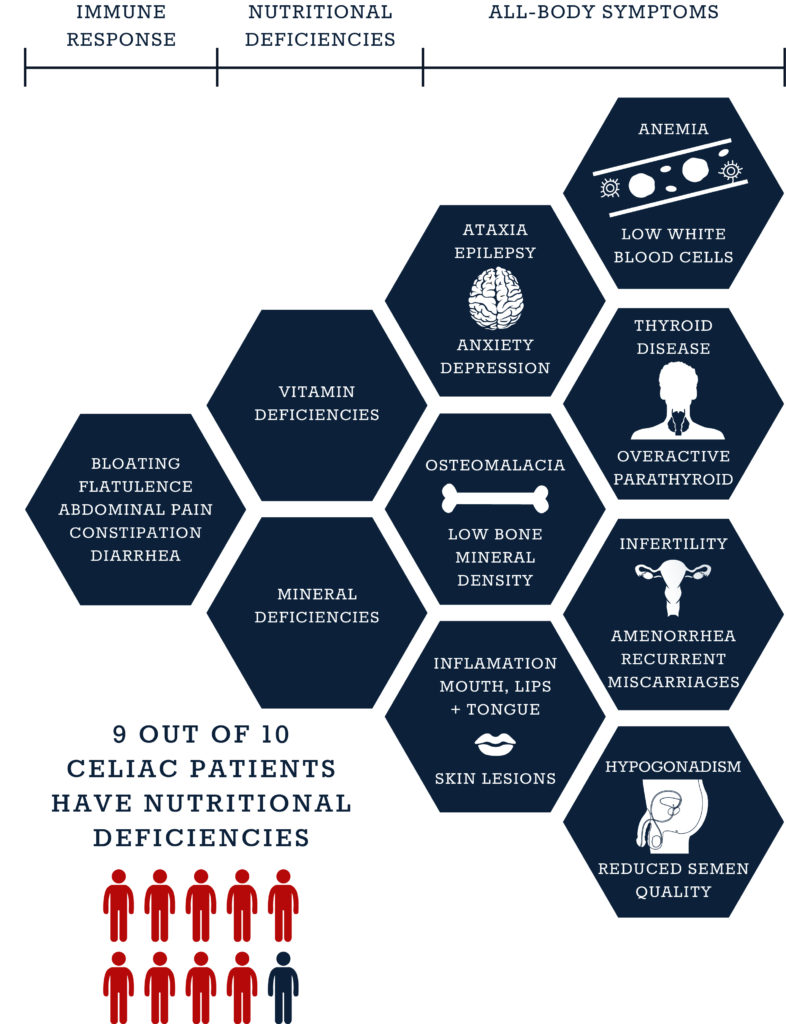
10 Categories of Celiac Symptoms and Their Causes
Celiac disease may be described as a condition affecting the digestive tract, but its reach extends from head to toe. Celiac disease is a remarkably difficult condition to diagnose. It may be tempting to blame the long list of symptoms, after all, there are more than 300 different signs and associated conditions, but this would be a massive understatement. To simplify and break down the hundreds of symptoms we have created 10 categories of celiac symptoms and their causes. The true challenge for diagnosis stems from the fact that this condition develops in a complex web of interlinked symptoms that is (almost) as unique to each patient as their own fingerprint.
When faced with seemingly unrelated symptoms, many not localized to the gastrointestinal tract and not exclusive to celiac disease, physicians need to work more like detectives “following clues” to get to the root of the problem: celiac disease.
The Immune response starts it all
It all starts in the gastrointestinal tract. Whether individuals develop symptoms or not, for celiac disease patients, the condition always starts with gluten in the diet, resulting in an immune response and inevitably damage to the lining of the intestine.
1. Localized immune response symptoms include (but are not limited to):
- abdominal pain and discomfort
- gassiness (flatulence) with bloating
- diarrhea or constipation
- heartburn
- Nausea and vomiting
Next follows nutritional deficiencies
Not surprisingly, this damage often leads to malabsorption, which in turn causes deficiencies in micronutrients, including vitamins and minerals. In fact, studies show that 9 out of 10 celiac disease patients have at least one nutritional deficiency at the time of diagnosis, and about half have more than one.
2. Symptoms due to malabsorption include (but are not limited to):
- Failure to thrive
- short stature and growth retardation
- Weight loss
- Anorexia
- Fatigue
- Water-soluble vitamin deficiencies (Vitamin B1, B2, B6, B12, vitamin K, and folic acid)
- Fat-soluble vitamin deficiencies (vitamin A, E and D)
- Mineral deficiencies (Iron, magnesium, zinc, manganese, calcium, potassium, copper and iodine)
Followed by the all-body symptoms
Finally, as a consequence of nutritional deficiencies, what started as a gastrointestinal condition soon manifests itself in a variety of unrelated symptoms spread throughout the body, from anemia to infertility. Celiac disease may be described as condition affecting the digestive tract, but its reach extends from head to toe.
In some cases, these extra intestinal manifestations overshadow the original symptoms and make for an even more complicated diagnosis. The symptoms of an immediate immune response caused by the presence of gluten are non-specific, therefore, doctors are more likely to diagnose celiac disease based on its nutritional deficiencies and subsequent symptoms.
Effects of deficiencies include, for example, iron, folic acid and vitamin K causing poor blood parameters and vitamin D and calcium depleting bone density, as well as selenium and iodine disturbing thyroid function and vitamin A, E and D causing infertility and other reproductive issues. A list of symptoms related to nutritional deficiencies that can be a part of celiac disease is as follows.
3. Neurological and psychiatric symptoms
- ataxia* (Vitamin E, Vitamin B3, B12)
- sensory neuropathy * (Vitamin E)
- impaired cognitive function
- psychiatric manifestations
- Epilepsy* (Folic acid)
- Dementia * (Vitamin B3)
- seizures * (Vitamin B3)
- headache
- difficulty concentrating
- depression
- schizophrenia
- anxiety
4. Musculoskeletal symptoms
- Osteomalacia * (Vitamin D, Calcium)
- osteoporosis* (Vitamin D, Calcium)
- low bone mineral density * (Zinc)
- muscular myopathies * (Vitamin E)
- Arthritis
5. Hepatic and renal symptoms
- Hypertransaminasemia (elevated transaminases)
- autoimmune liver disease
- primary biliary cirrhosis
- IgA nephropathy (kidney disease)
6. Dermatological symptoms
- Dermatitis herpetiformis
- loss of hair or fragile hair
- dermatomyositis (inflammation of the skin)
- urticaria
- itchy skin
- psoriasis
- inflammation of mouth and lips * (iron, vitamin B3, B12, folic acid)
- recurrent aphthous ulcers
- inflammation of the tongue * (Vitamin B group)
- Skin lesions * (Zinc)
7. Hematologic symptoms
- anemia * (Iron, folic acid, Vitamin B12, Copper)
- poor spleen function
- low white blood cells * (Vitamin B12, folic acid, Copper)
- low blood platelets * (Vitamin B12, folic acid, copper)
- Venous thrombosis
- Blood clotting disorders * (Vitamin K)
8. Endocrine and autoimmune symptoms
- Type 1 diabetes
- Thyroid disease * (Selenium, iodine)
- overactive parathyroid glands * (vitamin D, calcium)
- Sjogren’s syndrome (autoimmune disease in which the body destroys salivary and lacrimal glands)
- Addison’s disease (adrenal insufficiency)
- cardiomyopathy (heart disease)
- Lupus
9. Reproductive symptoms
- amenorrhea * (Zinc)
- infertility * (iron, folic acid, Vitamin B group)
- recurrent miscarriage * (iron, folic acid, vitamin B group)
- early menopause
- low pregnancy rate
- hypogonadism * (Zinc)
- impotence
- immature secondary sex traits
- reduced semen quality * (Vitamin A, E and D)
10. Oncological symptoms
- non-Hodgkin lymphoma
- small adenocarcinoma
- esophageal and oropharyngeal carcinoma
- T-cell lymphoma
Conclusion
From all these unrelated symptoms, there can only be an obvious conclusion: physicians should always bear in mind a possible celiac disease diagnosis and have a low threshold of suspicion for this condition. It may not explain every symptom associated with this condition, but the same way nutritional deficiencies may trigger a search for celiac disease, a diagnosis of celiac disease should prompt an immediate and extensive analysis assessing nutritional deficiencies. Typically, the best way to go forward in this situation is with adequate vitamin and mineral supplementation and close monitoring at follow-up appointments.
* may be caused by nutritional deficiencies as a consequence of malabsorption
This original article is made possible by Gluten Free Therapeutics. Our mission is to educate, inform, and provide the most effective nutritional products possible to allow those with celiac disease and serious gluten intolerances to heal their bodies. CeliVites complete line of superior gluten free supplements includes multivitamin/multimineral supplements, iron supplements, and calcium supplements for people living with celiac disease. All CeliVites products are designed to help you heal, restore and rebuild your body, because going gluten free isn’t enough!
REFERENCES
- Schuppan D, Zimmer KP. The diagnosis and treatment of celiac disease. Dtsch Arztebl Int. 2013 Dec 6;110(49):835-46.
- Fasano A, Catassi C. Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology. 2001;120:636–651
- Collin P, Kaukinen K, Välimäki M, Salmi J. Endocrinological disorders and celiac disease. Endocr Rev. 2002;23(4):464–483.
- Fasano A, Berti I, Gerarduzzi T, et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 2003;163(3):286–292
- Wierdsma NJ, Nijeboer P, de van der Schueren MA et al. Refractory celiac disease and EATL patients show severe malnutrition and malabsorption at diagnosis. Clin Nutr. 2015 Apr 30. pii: S0261-5614(15)00124-7.
- Salazar Quero JC, Espín Jaime B, Rodríguez Martínez A et al. Nutritional assessment of gluten-free diet. Is gluten-free diet deficient in some nutrient? An Pediatr (Barc). 2015 Jul;83(1):33-9.
- Dickey W, Ward M, Whittle CR et al. Homocysteine and related B-vitamin status in coeliac disease: Effects of gluten exclusion and histological recovery. Scand. J. Gastroenterol. 2008;43:682–688.
- Dahele A., Ghosh S. Vitamin B12 deficiency in untreated celiac disease. Am. J. Gastroenterol. 2001;96:745–750.
- Hallert C., Tobiasson P., Walan A. Serum folate determinations in tracing adult coeliacs. Scand. J. Gastroenterol. 1981;16:263–267.
- Stene-Larsen G., Mosvold J., Ly B. Selective vitamin B12 malabsorption in adult coeliac disease. Report on three cases with associated autoimmune diseases. Scand. J. Gastroenterol. 1988;23:1105–1108.
- Kemppainen T, Uusitupa M, Janatuinen E, et al. Intakes of nutrients and nutritional status in coeliac patients. Scand. J. Gastroenterol. 1995;30:575–579.
- Harper J, Holleran S, Ramakrishnan R, et al. Anemia in celiac disease is multifactorial in etiology. Am. J. Hematol. 2007;82:996–1000.
- Reinken L, Zieglauer H, Berger H. Vitamin B6 nutriture of children with acute celiac disease, celiac disease in remission, and of children with normal duodenal mucosa. Am. J. Clin. Nutr. 1976;29:750–753.
- Dickey W. Low serum vitamin B12 is common in coeliac disease and is not due to autoimmune gastritis. Eur. J. Gastroenterol. Hepatol. 2002;14:425–427
- Alwitry A. Vitamin A deficiency in coeliac disease. Br. J. Ophthalmol. 2000;84:1079–1080
- Henri-Bhargava A, Melmed C Glikstein R, Schipper H. Neurologic impairment due to vitamin E and copper deficiencies in celiac disease. Neurology. 2008;71:860–861
- Crofton R, Aggett P, Gvozdanovi S,et al. Zinc metabolism in celiac disease. Am. J. Clin. Nutr. 1990;52:379–382
- Hallert C, Grant C, Grehn S, et al. Evidence of poor vitamin status in coeliac patients on a gluten-free diet for 10 years. Aliment. Pharmacol. Ther. 2002;16:1333–1339.
- Wierdsma N, van Bokhorst-de van der Schueren M, Berkenpas M, et al. Vitamin and Mineral Deficiencies Are Highly Prevalent in Newly Diagnosed Celiac Disease Patients. Nutrients. 2013 Oct; 5(10): 3975–3992.
- Fasano A, Berti I, Gerarduzzi T, et al. Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med. 2003;163(3):286–292
- Bianchi ML, Bardella MT. Bone in celiac disease. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2008;19:1705–1716
- Ventura A, Magazzu G, Greco L. Duration of exposure to gluten and risk for autoimmune disorders in patients with celiac disease. SIGEP Study Group for Autoimmune Disorders in Celiac Disease. Gastroenterology. 1999;117:297–303
- Kane EV, Newton R, Roman E. Non-Hodgkin lymphoma and gluten-sensitive enteropathy: estimate of risk using meta-analyses. Cancer Causes Control. 2011
- Rubio-Tapia A, Kyle RA, Kaplan EL, et al. Increased prevalence and mortality in undiagnosed celiac disease. Gastroenterology. 2009;137:88–93
- Chin RL, Latov N. Peripheral neuropathy and celiac disease. Curr Treat Options Neurol 2005; 7: 43–48.
- Shams PN, Waldman A, Dogan A, et al. Ataxia in the setting of complicated enteropathy: double jeopardy. J Neurol Neurosurg Psychiatry. 2002;72(4):527–9.
- Cicarelli G, Della RG, Amboni M, et al. Clinical and neurological abnormalities in adult celiac disease. Neurol Sci. 2003;24(5):311–7
- Visakorpi JK, Kuitunen P, Pelkonen P. Intestinal malabsorption: a clinical study of 22 children over 2 years of age. Acta Paediatr Scand. 1970;59(3):273–80
- Freeman HJ. Pancreatic endocrine and exocrine changes in celiac disease. World J Gastroenterol. 2007;13(47):6344
- Hammans SR, Kennedy CR. Ataxia with isolated vitamin E deficiency presenting as mutation negative Friedreich’s ataxia. J Neurol Neurosurg Psychiatry. 1998;64(3):368–70
- Nikpour S. Neurological manifestations, diagnosis, and treatment of celiac disease: A comprehensive review. Iran J Neurol. 2012;11(2):59-64.
- Jameson S. Coeliac disease, insulin-like growth factor, bone mineral density, and zinc. Scand J Gastroenterol 2000; 35: 894–896.
- Devine A, Rosen C, Mohan S, Baylink D, Prince RL. Effects of zinc and other nutritional factors on insulin-like growth factor I and insulin-like growth factor-binding proteins in post-menopausal women. Am J Clin Nutr 1998; 68: 200–206.
- Lepore L, Martelossi S, Pennesi M, et al. Prevalence of celiac disease in patients with juvenile chronic arthritis. J Pediatr 1996; 129: 311–313
- Humbert P, Pelletier F, Dreno B, Puzenat E, Aubin F. Gluten intolerance and skin diseases. Eur J Dermatol 2006; 16: 4-11
- Gasbarrini G, Malandrino N, Giorgio V, et al. Celiac disease: what’s new about it? Dig Dis 2008; 26: 121-127
- Halfdanarson TR, Litzow MR, Murray JA. Hematologic manifestations of celiac disease. Blood 2007; 109: 412-421
- Green PH, Jabri B. Coeliac disease. Lancet 2003; 362: 383–391.
- Ozgör B, Selimoglu MA. Coeliac disease and reproductive disorders. Scand J Gastroenterol 2010; 45: 395-402.
Comments ()













I absolutely agree with the statement “physicians need to work more like detectives “following clues””…. That seems to be the problem (in the US). I suffered the symptoms from 6 years old to 40. NONE of the doctors I saw all those years ever gave me a correct diagnosis. And any time a “diet” was suggested it always contained gluten. And NONE of them even mentioned celiac or gluten. So after I self-diagnosed what was going on and took my self off of gluten (my symptoms visibly improved within 2 weeks) I returned to my doctor at the time for a routine check up and mentioned this to him. He response was arrogant, he said “Sure, it could be that. I’ve heard of it. But you really need to have a series of biopsies. YOU can’t diagnose yourself, that’s what I’m here for”. Really? The problem is doctors are human beings, which means that being greedy and lazy is in their nature. It seems that if a diagnosis will lead to an “easy” fix with no return visits a doctor won’t tell you.